Eczema Treatment in New York
Eczema Treatment NYC & Long Island
What Is The Main Cause of Eczema?
Eczema, also called atopic dermatitis, is a chronic inflammatory disorder of the skin. The cause of eczema is thought to be a genetic dysfunction in proteins that make up the epidermis. Inflammation is a complex process that normally protects the body’s cells against damage, but prolonged, unregulated inflammation, which occurs in eczema, is abnormal and harmful.
The skin condition affects the epidermis, the fifth and outermost layer of the skin that is in direct contact with the world. With eczema, the epidermis is irritated by the various triggers discussed below, and this irritation causes an inappropriately severe inflammatory response. That response leads to disruption of the skin’s normal function, as well as bothersome symptoms.
It is also a significant cosmetic concern and can be very upsetting psychologically. Double board-certified dermatologist, Dr. Rokhsar understands the frustration this skin condition can cause, and successfully treats eczema at his NYC and Long Island offices.
What are the symptoms of eczema?
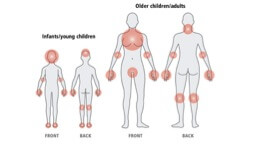
Eczema presents as a rash, chronically dry skin, pruritic (itchy) skin, and in some cases, lichenification (skin thickening) due to continuous scratching. In adults, the most common areas affected are the creases of the skin: the forearms, backs of the knees, inner surfaces of the wrists, ankles, and the neck.
How Can I Get Rid of Eczema?
Because it is is a chronic condition for which there is presently no cure, the goals of treatment are to alleviate symptoms, prevent future flare-ups, and address any cosmetic concerns. Symptom relief can be achieved by suppressing the over-stimulated immune system. This can be done using medications such as corticosteroids or topical immunosuppressants. Antihistamines can also be used to ease the uncomfortable feeling of constantly itchy skin.
Keeping the skin properly hydrated is an essential factor in controlling and treating atopic dermatitis in NYC. Contrary to popular belief, lotions, creams, and ointments are not all equally beneficial. Moisturizers with high water content are worse because the water evaporates and dries out the skin, which can actually stimulate outbreaks of eczema. Lotions contain the most water. The better options for skin moisturizers are creams or ointments: creams contain less water, and ointments contain none. This helps keep the epidermal layer intact.
What Triggers Eczema?
Being aware of what triggers eczema is important. People with eczema should try to avoid excessive heat (e.g., bathing in hot temperatures), excessive sweating, excessive bathing, emotional stress, anxiety, and low-humidity environments. This may seem frustrating at first, but it is possible to make slight lifestyle adjustments that will ease the pain of eczema.
Eczema Treatment in NYC
If you’re looking for eczema treatment in New York, you’ve come to the right place. Double board-certified dermatologist & laser surgeon, Dr. Rokhsar specializes in the treatment and prevention of eczema. We look forward to your visit!
Eczema FAQs
What does eczema look like?
Eczema is a common skin condition that can present differently in each individual. However, some common symptoms of eczema include dry, itchy, and inflamed skin with a rash that may appear as red, brown, gray, or purple patches. The affected area may also be swollen, scaly, flaky, or crusty. Eczema can occur anywhere on the body but commonly affects the arms, legs, and face. Sometimes, eczema can lead to thick, leathery patches of skin or small, coin-shaped lesions.
What causes eczema in babies?
Eczema in babies is a complex condition with no single cause. It is widely believed to be a result of a combination of genetic and environmental factors. Babies born to parents with eczema are more likely to develop the condition themselves, as it is hereditary. Eczema in babies can also be triggered by irritants and allergens in their environment, such as certain soaps, shampoos, and cleansers. Dry air and ointments can also trigger baby eczema. In addition, food allergies may also trigger eczema flares in some infants and young children.
The actual cause of eczema in babies is not fully understood, but some theories suggest that a dysfunction in the skin barrier may lead to skin dryness, which could trigger eczema. Another theory is that an overactive immune response to environmental factors may contribute to the development of eczema in babies.
What causes dyshidrotic eczema?
Dyshidrotic eczema, also known as pompholyx, is a chronic skin condition that affects the hands and feet. Although the exact cause of dyshidrotic eczema is unknown, several triggers have been identified, including contact with metals, wet hands or feet, allergies, and stress. Stress, in particular, can be a significant trigger for flare-ups in people with dyshidrotic eczema. Changes in weather, especially hot and humid conditions, can also trigger a flare-up. Dyshidrotic eczema typically affects adults between the ages of 20 to 40, and it’s twice as common in women as in men. If left untreated, dyshidrotic eczema can lead to secondary infections, paronychia, nail dystrophy, physical and psychological disability, and potential economic cost due to loss of work opportunity. If you suspect you have dyshidrotic eczema, it’s essential to seek medical advice from a board-certified dermatologist for proper diagnosis and treatment. Dr. Cameron Rokhsar is a double-board-certified Dermatologist and Dermatologic Surgeon, and he commonly treats patients for all kinds of eczema.
How long does eczema last?
Eczema is a chronic skin condition that causes dry, itchy, and inflamed skin. The duration of eczema flare-ups can vary depending on the type of eczema, its severity, and the health of the skin and its microbiome. Acute eczema may resolve completely after treatment, while chronic eczema may resolve and occasionally flare up again throughout your life. In general, eczema symptoms tend to last for a few weeks at a time, but eczema flares can last for two weeks or more, depending on what’s causing the flare. It’s important to identify the cause of the flare and treat it promptly to help get you to remission more quickly. Unfortunately, there’s no cure for eczema, but its symptoms can be managed with treatments like topical anti-inflammatory agents, topical corticosteroids, and phototherapy.
How to stop eczema?
First and foremost, it is important to keep the skin moisturized to prevent dryness, cracking, and itching. Using fragrance-free moisturizers, applying them regularly and within a few minutes of showering can help. Avoid harsh soaps and use mild ones, lukewarm showers, and avoid long baths.
Topical corticosteroids or calcineurin inhibitors can be prescribed to reduce inflammation and itching. Antihistamines can also be helpful in reducing itching and promoting sleep, especially when itching keeps you up at night. There are newer oral, injectable and topical treatments with new classes of drugs called Jak Inhibitors, or biologics which show great promise in treatment of severe eczema.
Additionally, if your eczema is severe, your doctor may suggest phototherapy or systemic medications, such as oral immunosuppressants or biologics. In some cases, a bleach bath may be recommended, however, it should only be done under medical supervision.
It is important to avoid triggers that can exacerbate eczema symptoms, including harsh chemicals, rough fabrics, and excessive heat or sweat. Identifying and avoiding these triggers can help prevent flare-ups.
How to treat eczema?
The first-line treatments for most cases of eczema are emollients and topical steroids. Emollients are moisturizers that help to soothe and hydrate dry, itchy skin, while topical steroids can help reduce inflammation and redness. In some cases, paste bandages and wet wraps may be added to the treatment plan to help manage severe itching and scratching.
For more severe cases of eczema, Dr. Rokhsar may recommend prescription-strength medications, such as immunosuppressants, antibiotics, or pills that control inflammation. It is important to work closely with your dermatologist to find the right treatment plan for you and to avoid using home remedies or over-the-counter treatments without medical guidance.
In addition to medical treatments, there are a variety of lifestyle changes that can help manage eczema symptoms. These include avoiding irritants and allergens, taking short, lukewarm baths, and using mild, fragrance-free soaps and detergents. It is also important to moisturize the skin regularly, wear loose-fitting clothing, and avoid scratching or rubbing the affected areas.
How to get rid of facial eczema?
Firstly, it is essential to maintain good hygiene practices and avoid further irritation caused by cosmetics and toiletries. Use a gentle cleanser and only fragrance-free and hypoallergenic cosmetics. Moisturizing your skin at least twice a day is crucial. Creams, ointments, shea butter, and lotions seal in moisture and can help reduce symptoms.
Topical steroids are commonly prescribed for facial eczema flares, while topical calcineurin inhibitors can be used for longer-term treatment and maintenance. Dr. Rokhsar may also prescribe antibiotic pills to treat an infection and pills that control inflammation for more severe eczema. Options might include cyclosporine, methotrexate, prednisone, mycophenolate, and azathioprine.
Other treatment options for facial eczema include using a lotion of 12% ammonium lactate or 10% alpha-hydroxy acid to help with flaky, dry skin, using medicated shampoos for dandruff, taking a dilute bleach bath, and applying mineral oil, peanut oil, or olive oil to the scalp. However, it’s always best to consult with a dermatologist to determine the best course of treatment for your specific case of facial eczema.
How to treat eczema on hands?
The first-line treatment for most cases of hand eczema is the regular use of emollients, which are moisturizers designed to hydrate and protect the skin. Topical steroids are another commonly used treatment, which can help reduce inflammation and itching. For more severe cases, doctors may prescribe systemic medications, such as oral steroids or immunosuppressants, to help control symptoms. In addition to these treatments, some people find success with phototherapy, paste bandages, or wet wraps. It is also essential to avoid triggers that can exacerbate eczema, such as irritants, allergens, and stress.
How to treat eczema on the scalp?
Treatment options for eczema on the scalp may include topical corticosteroids, calcineurin inhibitors, and antifungal agents. In some cases, phototherapy or systemic medications may be necessary.
In addition to medication, it is essential to maintain a regular scalp care routine. I advise against using harsh shampoos or hair products that may irritate the scalp. Instead, opt for gentle, fragrance-free products that are designed for sensitive skin. Regular washing of the scalp can help to remove excess oil, dirt, and buildup, which can contribute to inflammation.
It is also essential to avoid scratching the scalp as this can lead to further irritation and infection. If you experience itching, topical anti-itch creams containing hydrocortisone may be beneficial. However, these should only be used under the guidance of a board-certified dermatologist.
New York Office Locations
Upper East Side Manhattan Office
121 East 60th Street, Suite 8AB New York, NY 10022
(212) 285-1110
Long Island Office
901 Stewart Ave, Suite 240, Garden City, NY 11530
(516) 512-7616

 Dr. Rokhsar was chosen by
Dr. Rokhsar was chosen by